When adults develop blood cancer, they are frequently diagnosed with what is referred to as acute myeloid leukaemia.
The disease is triggered by pathological alterations of bone marrow cells, in which, in addition, an important mechanism is out of action: these cells do not die when they are damaged.
Researchers from the Technical University of Munich (TUM) have now discovered a molecular signalling pathway for self-destruction that is suppressed in leukaemia cells.
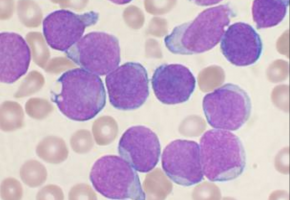
Leukaemia involves pathological alterations in the body's haematopoietic system.
In acute myeloid leukaemia, it is specifically the bone marrow (Greek: myelos) that is affected.
In a healthy body, different blood cells, which perform different functions in the blood, are formed from stem cells and what is referred to as progenitor cells in the bone marrow.
A genetic mutation can lead to alterations in stem cells and progenitor cells and turn them into leukaemia-initiating cells, which are referred to as LICs for short.
Like healthy progenitor cells, LICs multiply in the bone marrow.
The genetic mutation, however, causes LICs to remain without function and prevents them from developing into mature blood cells, which ultimately leads to the repression of healthy haematopoiesis in the bone marrow and the onset of leukaemia symptoms.
The most frequent genetic alterations in myeloid leukemia include mutations in the FLT3 gene.
A team led by Dr Philipp Jost from the Department of Hematology/Oncology at Klinikum rechts der Isar at the Technical University of Munich has now discovered that the effects of this gene on pathologically altered cells in a way provide certain indications for the treatment of the disease.
The mutation causes a permanent activation of the FLT3 gene.
As demonstrated by the scientists, this triggers inflammation-like stimuli in the cell, subjecting it to permanent stress.
Growth despite inflammation and damage
Under normal circumstances, such permanent inflammatory stimuli would trigger a program known as programmed cell death to replace damaged cells.
This is a kind of self-destruction mechanism used by a cell to initiate its own destruction in a coordinated fashion and allow it to be replaced by a healthy one.
"By contrast, LICs manage to grow and proliferate despite the inflammation and damage," states Philipp Jost.
"In our study, we have taken a closer look at the molecular causes of this resistance."
To gain a better understanding of the research project described by the TUM scientists in the medical journal Cancer Cell, it is important to understand that cells have different ways of self-destructing.
So far, the primary research focus in trying to ascertain why cancer cells survive longer than they should has been placed on a process called apoptosis.
However, the fact that inflammatory processes occur in LICs pointed Philipp Jost and his colleagues in a different direction.
Another way to initiate cell death is through what is referred to as necroptosis.
Whereas, in apoptosis, a cell shrinks in a coordinated fashion, in necroptosis, a sudden destruction occurs, which releases the contents of the dying cell along with numerous messenger substances.
This induces a strong inflammatory stimulus in the vicinity of the cell.
Cancer cells block activation of protein
Necroptosis is triggered by the activation of a protein called RIPK3, which subsequently initiates processes within the cell that lead to its death.
The scientists used cell cultures to discover that leukaemia takes a particularly severe course when RIPK3 is blocked inside LICs.
This led to the cancer cells surviving particularly long, accompanied by their strong division and conversion to functionless blood cells (blasts).
"We conclude from our findings that particularly aggressive cancer cells have the capacity to block RIPK3," states Ulrike Höckendorf, lead author of the study.
"Exactly how they accomplish this, however, remains to be investigated."
Inducing cell death in a LIC by means of necroptosis has repercussions which also affect neighbouring leukaemia cells.
The inflammatory stimuli triggered by the substances released during necroptosis are significantly stronger than the processes caused by the mutation in the FLT3 gene in a LIC.
This inflammation has positive effects on the area surrounding the cell: induced by the messenger substances, neighbouring leukaemia cells begin to mature similar to healthy cells, leading to a less aggressive progression of leukaemia.
With cell death blocked — apoptosis, too, is "neutralised" in many cancer cells— individual LICs manage to survive and proliferate even after chemotherapy or radiotherapy.
"The new findings on the impact of the RIPK3 signalling pathway and the messenger substances released could open up new options for the treatment of leukaemia," states Philipp Jost.
"If it were possible to artificially reproduce the effect of RIPK3 using medication, one could launch a targeted attack on leukaemia cells."
Source: Technical University of Munich
We are an independent charity and are not backed by a large company or society. We raise every penny ourselves to improve the standards of cancer care through education. You can help us continue our work to address inequalities in cancer care by making a donation.
Any donation, however small, contributes directly towards the costs of creating and sharing free oncology education.
Together we can get better outcomes for patients by tackling global inequalities in access to the results of cancer research.
Thank you for your support.