Interim analysis of a phase III study finds that adding the new anti-CD20 monoclonal antibody obinutuzumab to standard bendamustine chemotherapy significantly delays progression of indolent non-Hodgkin lymphoma (NHL).
Among patients for whom rituximab therapy no longer provided benefit, the average duration of remission was 29.2 months after receiving the new combination vs. 14 months after bendamustine alone.
The trial was stopped early based on these encouraging results.
“Unfortunately, there is yet no cure for indolent lymphoma, so the overall goal of treatment is to increase the amount of time patients remain symptom-free and in remission. The fact that this new approach doubled average remission time marks a major step forward for our patients,” said lead study author Laurie Helen Sehn, MD, MPH, a medical oncologist at the BC Cancer Agency in Vancouver, Canada.
“Obinutuzumab may offer patients the chance to stay well for a significantly longer period of time, putting off the need for additional chemotherapy.”
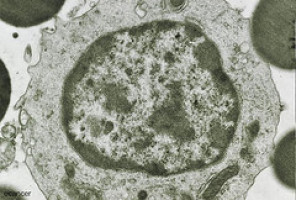
Indolent (slow-growing) NHL is a very common type of lymphoma.
The standard initial treatment for this disease is a combination of chemotherapy and the targeted drug rituximab.
The majority of patients ultimately become resistant to rituximab, and such patients have limited options for further treatment.
Obinutuzumab targets the CD20 protein, which is located on the surface of all B cells, including B-cell lymphoma cells.
Previous research suggested that when monoclonal antibodies attach to this protein, some lymphoma cells die, and others appear to become more sensitive to chemotherapy.
While obinutuzumab has been tested in smaller clinical trials in various types of lymphoma, this is the first randomised phase III trial to assess the potential benefit of obinutuzumab in patients with NHL.
The FDA has recently approved obinutuzumab in combination with chemotherapy for patients with chronic lymphocytic leukaemia.
The study included 396 patients with various types of NHL, the most common being follicular lymphoma.
The patients were randomly assigned to treatment with bendamustine alone or a combination of bendamustine and obinutuzumab followed by obinutuzumab single-agent therapy.
After an average follow-up of 21 months, the median investigator-assessed progression-free survival was 14 months for bendamustine alone vs. 29.2 months for the combination arm.
The median progression-free survival by independent review has not been reached.
Dr. Sehn noted that longer follow-up is needed to determine the potential overall survival benefit associated with obinutuzumab.
In general, there were no unexpected side effects or safety concerns from the combination regimen.
Low white blood cell counts and infusion-related reactions were slightly more frequent in the combination arm compared to the bendamustine arm.
The rates of low platelet counts, anaemia and pneumonia were higher in the bendamustine alone arm.
Watch the press conference for more.
Source: ASCO
We are an independent charity and are not backed by a large company or society. We raise every penny ourselves to improve the standards of cancer care through education. You can help us continue our work to address inequalities in cancer care by making a donation.
Any donation, however small, contributes directly towards the costs of creating and sharing free oncology education.
Together we can get better outcomes for patients by tackling global inequalities in access to the results of cancer research.
Thank you for your support.