Measurement of circulating tumour DNA (ctDNA) in blood can be used to detect disease recurrence in patients with a curable form of cancer known as diffuse large B-cell lymphoma (DLBCL).
In most patients, measurement of ctDNA enabled detection of microscopic disease before it could be seen on computerised tomography (CT) scans, which is the current standard for disease assessment.
Monitoring for recurrence by testing blood samples may reduce the need for multiple CT scans that increase a patient’s exposure to radiation and add to health care costs.
Advances in the ability to monitor for disease recurrence earlier may also improve the ability of physicians to successfully treat the disease at the time recurrence is diagnosed.
This research was conducted by investigators at the National Cancer Institute (NCI), part of the National Institutes of Health, and appeared April 2, 2015, in Lancet Oncology.
DLBCL is usually curable, but when treatment fails, the long-term prognosis is poor.
Currently, imaging using CT or interim PET (iPET) scans is used to monitor patients during and after treatment, but is often imprecise.
Repeated radiation exposure is a potential health risk and a financial burden.
Because relapses of DLBCL most likely occur due to the presence of residual disease at a level below that which can be detected by imaging, a more precise measure of disease recurrence potential was sought.
NCI investigators, led by Wyndham Wilson, M.D, Ph.D, Center for Cancer Research, analysed serum from 126 patients with DLBCL for the presence of ctDNA.
To detect ctDNA in serum, the researchers used a quantitative method that assesses gene segments with advanced sequencing techniques.
All patients received therapy involving the drugs etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin, known as EPOCH, with or without the biologic agent rituximab, in clinical trials between May 1993 and June 2013.
Serum samples were collected before treatment, during treatment, and for many years after therapy.
The patients also had CT scans done at the same time as the blood testing as part of standard surveillance.
They were followed for a median of 11 years after the completion of therapy.
Results of this study showed that, among the 107 patients who achieved complete remission, those who developed detectable ctDNA during surveillance were over 200 times more likely to have their disease progress than those who did not have detectable ctDNA.
The researchers also found that measuring ctDNA enabled the detection of cancer recurrence a median of 3.5 months before clinical evidence of disease.
In addition, the ctDNA test was able to predict which patients would not respond to therapy as early as their second cycle of treatment, a strategy known as interim monitoring.
“Interim ctDNA is therefore a promising biomarker to identify patients at high risk of not responding to treatment for their disease,” noted Dr. Wilson.
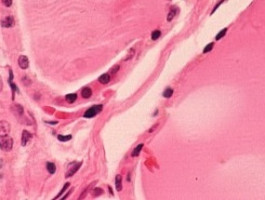
DLBCL is the most common type of lymphoma, a cancer that arises in the lymphatic system, where infection-fighting cells are generated.
Most people with this cancer show no signs of disease after their initial therapy, but, because of the risk of recurrence, they currently undergo imaging by CT scanning on a regular basis for up to five years after their initial disease remission.
However, the disease recurs in up to 40 percent of patients and is then often incurable, particularly in those who progress early and/or have significant levels of tumour cells in their blood.
“Even with frequent CT imaging, administered for a median of 11 times per patient in our study, early disease detection was suboptimal. Indeed, a recent study suggested that surveillance CT scans might be no better than an up-to-date patient history and physical exams, supporting the need for more effective monitoring technologies,” said Dr Wilson.
The patients in this study did not undergo iPET scanning, but the researchers noted that it would be of interest to compare interim ctDNA monitoring and iPET in future clinical studies.
The researchers also suggested that for patients with newly diagnosed DLBCL, early disease detection based on ctDNA could be employed as a biomarker to test novel targeted agents with the monitoring of response at the molecular level.
Source: National Cancer Institute
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.