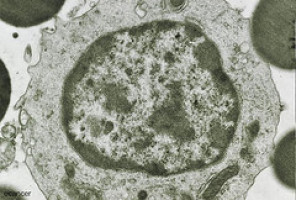
Classical Hodgkin lymphoma (cHL) is characterised by a genetic alteration that likely supports cancer growth by manipulating a common immune pathway called the PD1 pathway.
This alteration results in increased engagement of PD-1, a receptor on the surface of immune cells, dampening the immune response to the cancerous cells.
Researchers evaluating this unique interaction hypothesised that blocking the PD-1 signal from reaching the immune cells might restore their cancer-fighting power.
Nivolumab for Hodgkin lymphoma
To help determine whether blocking PD-1 activity could be a safe and effective way to treat cHL, investigators conducted a Phase I study of the PD-1 inhibitor nivolumab in 23 patients with relapsed or resistant cHL, 87 percent of whom had failed more than three previous treatment regimens, including stem cell transplant and brentuximab vedotin.
Patients received an intravenous infusion of nivolumab every two weeks until their tumours progressed or they experienced excessive toxicity. At the time of the latest analysis in June 2014, and after an average follow up of 40 weeks, 20 of 23 patients (87%) receiving nivolumab had experienced either complete response (four patients, 17%) or partial response (16 patients, 70%).
The drug’s toxicity mirrored that observed in other solid tumour cancers, with no life-threatening toxicity, and 22 percent of patients experiencing a serious treatment-related adverse event. Based on these results, the U.S. Food and Drug Administration has granted nivolumab breakthrough therapy designation in relapsed cHL, and a large, multi-national Phase II study is underway.
“Our data are encouraging for Hodgkin lymphoma patients with relapsed or treatment-resistant disease, and the remarkable response rate seen in this study validates the scientific hypothesis that Hodgkin lymphoma relies heavily on the PD-1 pathway for survival,” said lead study author Philippe Armand, MD, PhD, of Dana-Farber Cancer Institute in Boston.
“We hope that further development of this drug can lead to improved outcomes for patients afflicted with this cancer.”
Watch the interview and the press conference here.
A new role for pembrolizumab
Pembrolizumab is a PD-1 inhibitor in the family of checkpoint inhibitor drugs already approved for melanoma and now under development to support the immune system in fighting classical Hodgkin lymphoma.
This Phase 1 study evaluated the PD-1 inhibitor pembrolizumab in 29 heavily pre-treated patients with cHL. All patients in this study failed previous treatment with brentuximab vedotin, and 69 percent of patients enrolled had relapsed after a stem cell transplant. Patients received pembrolizumab intravenously every two weeks until disease progression, excessive toxicity, or completion of two years of therapy.
At the time of analysis in November 2014, 66 percent of the patients responded to the drug, with six patients (21%) achieving a complete remission and 13 patients (45%) achieving a partial remission.
Pembrolizumab appeared to be well-tolerated, as there were no serious treatment-related adverse events, and only three patients experienced moderate treatment-related adverse events.
“These results are particularly compelling since they are demonstrating complete responses to a drug in a patient population who had failed all other therapies; this was their last chance,” said lead study author Craig Moskowitz, MD, of Memorial Sloan Kettering Cancer Centre in New York.
“It will be important to further evaluate this drug in combination with others, or perhaps even as a maintenance treatment, to enhance the post-transplant immune response.”
Watch the interview and the press conference here.
Source: ASH
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.