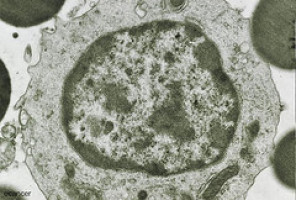
Patients with chronic lymphoid leukaemia (CLL) or small lymphocytic lymphoma (SLL) who experience short response duration or adverse cytogenetics have poor outcomes.
Dr Peter Hillmen (St. James’s Institute of Oncology, Leeds, UK) et al evaluated the efficacy of ibrutinib, the first-in covalent inhibitor of Bruton's tyrosine kinase, in these difficult-to-treat patients.
This multicentre, international, phase 3 study (RESONATE™) assessed daily ibrutinib monotherapy versus the anti-CD20 antibody ofatumumab.
Relapsed or refractory CLL/SLL patients (N=391) were randomised to receive ibrutinib or ofatumumab.
At a median follow-up of 9.4 months, ibrutinib significantly improved progression free survival (PFS); median PFS was not reached with ibrutinib and was 8.1 months with ofatumumab (hazard ratio [HR], 0.22; P<0.001).
Ibrutinib also significantly improved overall survival (HR, 0.43; P=0.005).
This effect was observed despite cross over from ofatumumab to ibrutinib at progression as recommended by the data monitoring committee.
Similar effects were observed regardless of del17p or purine analogue-refractory disease.
The Response rate by IRC was 63% for ibrutinib including 20% responses with lymphocytosis vs. 4% with ofatumumab.
Toxicities were manageable and did not frequently result in dose reduction or treatment discontinuation with 86.4% continuing ibrutinib at time of analysis.
In summary, ibrutinib significantly improved PFS, overall survival, and response rate compared to ofatumumab in previously treated CLL/SLL.
This study validates ibrutinib as an effective new single agent therapy for CLL/SLL patients.
Source: EHA
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.