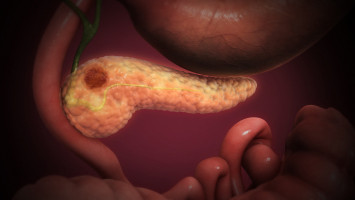
Pancreatic cancer is among the deadliest forms of cancer, with most patients diagnosed after the disease has already spread throughout the body.
The five-year survival rate for metastatic cases hovers around 2–3%, and median survival is often measured in months rather than years.
Now, UCLA researchers have engineered a novel immunotherapy that could offer new hope for a disease that has remained stubbornly resistant to treatment advances for decades.
In a study published in PNAS, the team details how the therapy, called CAR-NKT cell therapy, can track down and destroy pancreatic tumours even after they’ve metastasised to other organs.
“Developing a therapy that targets both the primary tumour and its metastases in preclinical studies — one that can be ready to use off-the-shelf — represents a fundamental shift in how we might treat this disease,” said senior author Dr. Lili Yang, a professor of microbiology, immunology and molecular genetics and a member of the Eli and Edythe Broad Centre of Regenerative Medicine and Stem Cell Research at UCLA.
The therapy uses engineered immune cells that can be mass-produced from donated blood stem cells and stored ready-to-use.
This approach offers an immediately available treatment option at approximately $5,000 per dose — a fraction of the cost of current personalised cell therapies, which can run hundreds of thousands of dollars and require weeks of manufacturing time that many pancreatic cancer patients simply don’t have.
Breaching the cancer fortress
CAR-T cell therapies have revolutionised treatment for certain blood cancers, but they’ve struggled against solid tumours like pancreatic cancer.
Pancreatic tumours build a dense protective barrier of connective tissue and suppressive immune cells that block therapeutic cells from reaching the cancer.
Even more challenging, these tumours are masters of disguise, constantly changing their molecular markers to evade detection.
To overcome these obstacles, Yang’s team harnesses a rare but powerful type of immune cell called invariant natural killer T cells, or NKT cells.
When equipped with a chimaeric antigen receptor, or CAR, targeting mesothelin — a protein found on pancreatic cancer cells — these cells gain the ability to attack tumours through multiple independent mechanisms simultaneously.
“We’re essentially surrounding the tumour with no escape routes,” said first author Dr. Yanruide (Charlie) Li, a postdoctoral scholar in the UCLA Broad Stem Cell Research Centre Training Programme. “Even when the cancer tries to evade one attack pathway by changing its molecular signature, our therapy is hitting it from multiple other angles at the same time. The tumour simply can’t adapt fast enough.”
Reaching tumours wherever they spread
One of the most challenging aspects of metastatic pancreatic cancer is that disseminated tumours in the lungs and liver are notoriously difficult for immune cells to reach and infiltrate.
Conventional CAR-T cells often get blocked outside tumour sites, unable to penetrate the dense tissue barriers.
The UCLA team tested their therapy using advanced preclinical models specifically designed to mimic the harsh conditions of human pancreatic cancer — a critical step that sets a higher bar for success than standard testing approaches.
“Many treatments that looked promising in simpler lab models have completely failed in patients,” said study collaborator Dr. Caius Radu, a UCLA professor of molecular and medical pharmacology.
“We used orthotopic models where tumours grow in the pancreas itself, and metastatic models targeting the liver, which is one of the most common and deadly sites of spread. The fact that this therapy worked in both settings is genuinely encouraging.”
In these rigorous tests, the CAR-NKT cells demonstrated remarkable tumour-homing abilities.
“These cells express high levels of chemokine receptors — molecular GPS systems that guide them directly to tumour sites,” Li said.
When the tumour is in the lung, they go to the lung. When it’s in the pancreas, they go to the pancreas. They actively seek out and infiltrate the cancer wherever it’s hiding.”
When tested across different mouse models of pancreatic cancer, including tumours growing in the pancreas, tumours that had spread to other organs and tumours grown under the skin, the therapy consistently slowed tumour growth and extended survival.
The therapeutic cells maintained their cancer-killing potency even in the harsh, inflammatory tumour environment and showed minimal signs of exhaustion, a common problem that causes other cell therapies to lose effectiveness over time.
Engineering universal accessibility
Beyond its multipronged cancer-fighting capabilities, the platform addresses key barriers that have limited cell therapy access: time, manufacturing complexity and cost.
Current cell immunotherapies involve collecting each patient’s immune cells, sending them to specialised facilities for genetic modification, then returning the modified cells back into the patient weeks later.
For patients battling pancreatic cancer, particularly those in advanced stages, a treatment delay of several weeks can be devastating.
Yang’s team takes a fundamentally different approach.
Since NKT cells are naturally compatible with any immune system without causing dangerous rejection reactions, they can be mass-produced from donated blood stem cells using a scalable system.
One donor could provide sufficient cells for thousands of treatments.
One product to fight multiple cancers
Since the therapy targets mesothelin — a protein also highly expressed in breast, ovarian and lung cancers — the same cell product could potentially treat multiple cancer types.
The team has already demonstrated the therapy’s effectiveness against triple-negative breast cancer and ovarian cancer in separate preclinical studies.
“We hear from people almost every day wanting to know if our new cell therapy can help treat their loved ones,” Li said.
“Meeting this critical unmet medical need is what drives us.”
With all preclinical studies now complete, the team is preparing to submit applications to the Food and Drug Administration to begin clinical trials.
“Pancreatic cancer patients need better treatment options now,” said Yang, who’s also a member of the UCLA Health Jonsson Comprehensive Cancer Centre. “We’ve developed a therapy that’s potent, safe, scalable and affordable. The next critical step is proving it can deliver the same results in patients that we’ve seen in our preclinical work.”