A new study from the University of Michigan Rogel Health Cancer Centre, published in Science, sheds light on how two distinct classes of mutations in the FOXA1 gene—commonly altered in prostate cancer—drive tumour initiation formation and therapeutic resistance.
FOXA1, a key transcription factor that facilitates androgen receptor binding to DNA, is mutated in 10–40% of hormone-dependent prostate cancers.
While common, the exact ways these mutations alter cancer cells have remained elusive—until now.
Rogel researchers, including Arul Chinnaiyan, M.D., Ph.D., S.P.Hicks Endowed Professor of Pathology and Urology, and Abhijit Parolia, Ph.D., Rogel Fellow and Assistant Professor of Pathology, used mouse models to understand the mechanisms underlying two major classes of FOXA1 mutations.
In addition to establishing FOXA1 as a true oncogenic driver in prostate cancer, their findings reveal the distinct ways that each class of FOXA1 mutations operate.
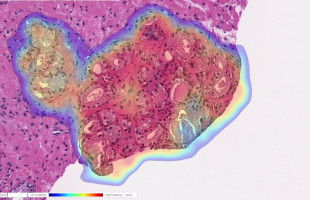
Firstly, Class 1 mutations, commonly observed in primary prostate cancer, work with loss of the gene TP53 to promote the formation of aggressive tumours.
Like human prostate cancer, tumours in the mouse models retain hormone sensitivity and shrink in response to androgen deprivation therapy.
Alternatively, Class 2 mutations, typically found in metastatic prostate cancer, do not independently initiate tumour growth.
Instead, they reprogram the cellular lineage identity, driving resistance to hormonal therapies.
“This is the first in vivo demonstration of FOXA1 as an initiator of prostate cancer,” said Chinnaiyan.
“Prior studies relied on cell lines, but our mouse models provide definitive evidence of its causal role in tumour development.”
These insights build on earlier work that categorised three major FOXA1 mutation types.
“This study goes further,” Chinnaiyan added, “by revealing how distinct alterations within the same gene can initiate disease in early stages or confer resistance in late-stage, therapy-refractory tumours.”
Hormone therapy is central to prostate cancer treatment.
Though initially effective, most patients develop resistance to androgen deprivation therapy, leading to incurable disease.
“Modelling primary prostate cancer’s response to androgen withdrawal in mouse models has been challenging” said Parolia.
“We demonstrated that prostate tumours driven by Class 1 mutations require continuous androgen supply for growth and survival, establishing the FOXA1/p53 mouse model as a valuable preclinical system.”
In metastatic disease, Class 2 mutants acquire the ability to access latent DNA sites.
“Activation of these sites turn on genes that drive adaptation to androgen blockade, enabling cancer’s escape from therapy,” Parolia explained.
The team’s findings reveal two faces of the FOXA1 oncogene and deepen understanding of prostate cancer evolution, while opening potential avenues for FOXA1 mutation-specific therapeutic strategies.
Source: Michigan Medicine - University of Michigan
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.