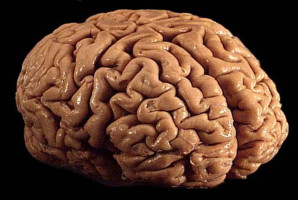
A multidisciplinary team of University of Cincinnati Cancer Center researchers have opened a phase 2 clinical trial to test a new combination treatment for glioblastomas (GBM), the most deadly form of brain tumours.
The team, led by UC’s Pankaj Desai, PhD, and Trisha Wise-Draper, MD, PhD, has been awarded a Catalyst Research Award from the Dr. Ralph and Marian Falk Medical Research Trust to move the trial forward.
Study background
Difficult to diagnose at early stages, GBMs are aggressive brain tumours that become symptomatic once the tumour is substantial. Current treatments include immediate surgery to safely remove as much tumour as possible, radiation and chemotherapy, but the tumour often recurs or becomes resistant to treatments. The average patient survives no more than 15 months after diagnosis.
Drug-based treatments for GBMs face an additional challenge known as the blood-brain barrier, which only allows certain compounds into the brain based on their physical and chemical properties.
The research team is focused on the use of a drug called letrozole that has been used for more than 20 years as a treatment for breast cancer. The drug targets an enzyme called aromatase that is present in the breast cancer cells and helps the cells grow.
Early research in Desai’s lab found that aromatase was present in brain tumour cells, making letrozole a potential new treatment for GBMs.
Phase 0/1 trial results
To bring letrozole from Desai’s lab to patients’ bedsides, he collaborated with Wise-Draper and neuro-oncologists and neurosurgeons at UC’s Brain Tumor Center to launch a Phase 0/1 clinical trial.
“In the academic setting, we are very good at doing molecular research that enhances our understanding of the mechanism of disease and preclinical characterization of efficacy, safety and other aspects of drug development research,” said Desai, professor and chair of the Pharmaceutical Sciences Division and director of the drug development graduate program in UC’s James L. Winkle College of Pharmacy. “But you can’t translate this into a clinical trial without a Phase 1 clinical trial expert like Dr. Wise-Draper and the experts at the Brain Tumor Center.”
The researchers published the results of the Phase 0/1 trial in Clinical Cancer Research, a journal of the American Association for Cancer Research.
“Letrozole was safe up to the highest dose, and there were no safety concerns in the Phase 0/1 trial,” said Wise-Draper, section head of Medical Oncology and professor in the Division of Hematology/Oncology in UC’s College of Medicine. “The biggest conclusion is that it was safe and that we could reach what we felt was going to be the effective dose based on Dr. Desai’s preclinical work.”
The research team collected tumour tissues from patients enrolled in the Phase 0/1 trial and found that letrozole was crossing the blood-brain barrier when they analyzed the samples in Desai’s lab.
“We can categorically show that in humans the drug actually crosses and reaches the brain tumour at concentrations that we believe are likely to be most efficacious,” Desai said.
Phase 2 trial design
Since GBMs are aggressive and complicated tumours, Desai said most likely new effective treatments will be combinations of drugs instead of one single drug.
In the Phase 2 trial, patients will be given letrozole in combination with a chemotherapy drug called temozolomide that is already approved as a GBM treatment. Desai said preclinical research in his lab and input from Brain Tumor Center collaborators, including neuro-oncologist and former UC faculty member Soma Sengupta, suggested this combination treatment could be more effective than letrozole alone.
A total of 19 patients with recurrent GBM who are no longer eligible for additional surgery will be enrolled in the first stage of the trial. The results from this trial will guide the design of future larger Phase 2 trials.
The team estimates it will complete enrollment within two years, and two patients have already been enrolled.
Collaboration and funding support
Wise-Draper and Desai have worked together on various research projects for nearly 15 years and said this project would not be moving forward without the varied expertise each team member brings.
“I think collaboration with multidisciplinary teams is critical to be able to have the expertise and all the components you need, including biostatistics, pharmacokinetics, clinical, basic science and neuro-oncology expertise,” Wise-Draper said. “The future of all science is team science. No one really can do everything on their own anymore because we’re all too specialized.”
“Only academic centers with integrated scientific and clinical expertise are able to move their molecules from the research bench to clinical trials,” Desai added. “It takes a lot of persistence, ups and downs, highs and lows of funding, but we have been supported by a very strong team of people. It’s a journey that has taken a while and a lot of hard work by a number of people, and we’re in a very exciting stage.”
Early-stage support for the preclinical and clinical trial studies was provided by the UC Brain Tumor Center, where investigators from UC’s colleges of Medicine, Pharmacy, Engineering and Applied Science and Cincinnati Children’s Hospital collaborate on brain tumor research.
UC’s Brain Tumor Center provided direct support for the completion of the Phase 0/1 trial and some of the correlative mechanistic studies that will continue during the Phase 2 trials using funds raised in the annual Walk Ahead for a Brain Tumor Discoveries fundraiser.
The Falk Catalyst Award provides up to $350,000 in seed funding to support translational research projects, which the researchers said was crucial in opening the new trial.
“Oftentimes the funding is somewhat limited for initial clinical trial development compared to many other more early-stage studies that you can do,” Desai said. “So that gap is filled by foundations like the Falk Medical Research Trust, and that really is very helpful and plays a critical role in accelerating clinical development.”
“It would not be possible if we didn’t have the funding to be able to bring this combination into patients that desperately need new treatment options,” Wise-Draper said.
As the clinical trial progresses, the team is also collaborating to find other drugs to combine with letrozole to treat GBMs, funded by a $1.19 million National Institutes of Health/National Institute of Neurological Disorders and Stroke grant. The team is already preparing a proposal for larger confirmatory Phase 2 studies and expanding the opportunities for cutting-edge brain tumour clinical trials in Cincinnati.
Desai said the ongoing research includes additional collaboration from experts including David Plas, PhD, Biplab DasGupta, PhD, and Tim Phoenix, PhD (molecular/cancer biology); Gary Gudelsky, PhD (neuro-pharmacology) Rekha Chaudhary, MD, and Lalanthica Yogendran, MD (neuro-oncology); Mario Medvedovic, PhD (bioinformatics and genomics); and Shesh Rai, PhD (biostatistics). Many graduate students, postdoctoral fellows and the clinical trials support staff also provide essential support for the project.
Source: University of Cincinnati
We are an independent charity and are not backed by a large company or society. We raise every penny ourselves to improve the standards of cancer care through education. You can help us continue our work to address inequalities in cancer care by making a donation.
Any donation, however small, contributes directly towards the costs of creating and sharing free oncology education.
Together we can get better outcomes for patients by tackling global inequalities in access to the results of cancer research.
Thank you for your support.