A clinical trial from Keck Medicine of USC aims to provide a surgical solution for patients with a form of advanced pancreatic cancer previously considered inoperable.
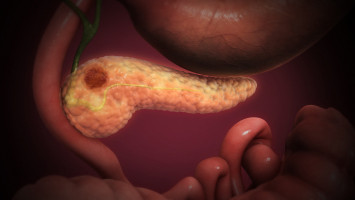
The study will investigate if chemotherapy followed by a novel type of surgery to remove the cancer is a safe and effective option for patients with locally advanced pancreatic cancer, meaning that the cancer has not spread to other organs, but has grown into or close to nearby blood vessels that surround the pancreas.
“Usually, these types of tumours cannot be safely removed with surgery because of the risk of damaging the blood vessels, which supply blood to the stomach, liver and other abdominal organs. However, due to recent advancements by Keck Medicine surgeons, we believe that patients with locally advanced cancer can be candidates for successful surgery, which could significantly improve outcomes,” said Steven Grossman, MD, PhD, co-lead investigator of the study. Grossman is a medical oncologist with Keck Medicine and deputy director for cancer services at USC Norris Comprehensive Cancer Center, part of Keck Medicine.
The challenge of treating pancreatic cancer
Pancreatic cancer accounts for only about 3% of cancers in the United States, but it is one of the deadliest. People usually have no symptoms until the cancer has become very large or metastasised throughout the body, so the cancer is caught late, and patients have poor prognoses.
Only 13% of pancreatic cancer patients survive five or more years after diagnosis.
The life expectancy of patients with locally advanced pancreatic cancer, which accounts for one-third of all pancreatic cancer cases, has historically been about one year.
For most forms of cancer, surgery is considered the most effective treatment for localised tumours that have not spread to other areas of the body. However, surgery has traditionally not been offered for tumours involving the blood vessels near the pancreas because if the blood vessels were to become damaged during the procedure, and the blood flow to organs interrupted, it could result in serious side effects or death.
Therefore, typically the only treatment option for patients with locally advanced cancer is chemotherapy and/or radiation, both of which have limited effectiveness killing pancreatic cancer cells.
“The situation is frustrating because research shows that in the rare cases where locally advanced tumours were safely removed, the progression of the disease was slowed and the patient’s length of survival on average increased from one year to 28 months, more than doubling life expectancy,” said Sandra Algaze, MD, a medical oncologist with Keck Medicine, a member of USC Norris and one of the study’s investigators. “Surgery, therefore, appears to strongly benefit a patient’s survival rate, which is why the medical field has been eager for a surgical solution.”
How new surgical advances can benefit patients
The clinical trial will use surgical protocols pioneered by Keck Medicine surgeons to safely remove locally advanced pancreatic tumours attached to arteries. The surgical team will be led by study co-lead investigator Yuri Genyk, MD, a hepatobiliary and pancreatic surgeon with Keck Medicine who is an expert in vascular reconstruction, which is the removal and reconstruction of blood vessels. Genyk has already successfully removed about 30 pancreatic tumours that were attached to adjacent arteries.
“While this surgery is very complex, we have the skills and expertise to execute it and train other skilled surgeons in the procedure. If the trial results are positive, we envision that the technique could become the gold standard for how this stage of pancreatic cancer is treated in the future,” said Genyk.
Patients in the clinical trial will first undergo chemotherapy to attempt to shrink the tumour. Two to eight weeks after completing chemotherapy, they will undergo a laparoscopic evaluation to determine the position and size of the tumour before the tumour is surgically removed and involved blood vessels are removed and reconstructed.
Patients will be followed every three months for the first year post-surgery and then every six months for two years after that.
The clinical trial will also examine if certain biomarkers, such as the tumour’s DNA, as well as a patient’s demographic factors such as age and gender, play a role in patient outcomes.
The study hopes to enroll 20 patients with locally advanced pancreatic cancer who have evidence of arterial involvement by their tumours. The surgeries will be performed at Keck Hospital of USC.
“Pancreatic cancer is a devastating diagnosis, and Keck Medicine is committed to finding better solutions for the disease,” said Grossman. “Anything we can do to improve patients’ quality of life and extend life expectancy will be a huge milestone that could benefit countless patients and their loved ones.”
Source: Keck Medicine of USC