Findings
Scientists at City of Hope, one of the largest cancer research and treatment organisations in the United States, have devised an innovative approach to target and destroy hard-to-kill leukaemia stem cells.
The journal Blood published the preclinical findings.
By overcoming challenges, such as drug resistance and treatment relapse common to patients with acute myeloid leukaemia (AML), the therapy method could provide a less toxic and more effective approach for older and sicker patients who don’t quality for stem cell transplants — currently the only cure for AML available.
Type II interferon (IFNy), a substance produced by immune cells, disrupts the leukaemia stem cells’ ability to divide and spread cancer.
However, IFNy also stimulates CD38, a protein that suppresses the immune cells’ ability to mount a response against infection.
To overcome this challenge, the researchers designed a T cell engager antibody called CD38-BIONIC that creates a bridge between the T cells and the leukaemia stem cells expressing CD38, enabling the immune system to kill off the cancer cells.
Equally important, the approach did not damage healthy early blood stem cells or immune cells in human tissue or AML mouse models.
Significance
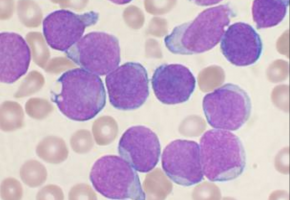
When leukaemia invades the bone marrow, it produces abnormal early blood cells called blasts that are CD38-positive.
These divide rapidly and are easy to target. In contrast, the leukaemia stem cells that form cancer stubbornly resist treatment and are CD38-negative.
“CD38 has successfully been exploited as a therapeutic target in multiple myeloma and other forms of leukaemia,” said Flavia Pichiorri, Ph.D., M.S., who co-led the study with fellow investigators John Williams, Ph.D., and Guido Marcucci, M.D. — all professors at City of Hope.
“Because AML stem cells are mainly CD38-negative, however, scientists have not prioritised CD38 as a therapeutic target for relapsed acute myeloid leukaemia.”
In the current study, CD38-BIONIC binds to the CD38-positive blasts.
This triggers the T cells to release IFNy, which converts the immature leukaemia stem cells from CD38-negative to CD38-positive.
In one stroke, the engineered antibody unmasks all the leukaemia cells, exposing them to treatment.
“We believe that the compact format of BIONIC leads to an efficient immune system connection point with the CD38-positive blast, which drives IFNy production,” said Williams.
“The leukemia stem cells react to the IFNy, painting themselves with CD38, which in turn allows them to be targeted by the CD38-CD3 BIONIC.”
Marcucci added, “This novel mechanism and the targeting by City of Hope’s homegrown approach will allow us to eliminate otherwise dormant leukaemia stem cells. Our hope and goal is that eradication of leukaemia stem cells will decrease and even eliminate the risk of disease relapse in patients with AML, but much more research needs to be done to translate our preclinical research into human treatment.”
Background
Despite recent Food and Drug Administration-approved therapies, only 30% of adult patients with AML survive five years past diagnosis.
More than half of patients relapse after treatment, and treatment resistance remains a major challenge.
Patients often must remain hospitalised because their blood and immune systems are compromised by the cancer and its therapies.
While stem cell transplants from a bone marrow donor can prolong life, many older patients do not qualify due to their compromised health or the inability to find a matched donor.
The majority of patients with AML urgently need less toxic and more effective treatments.
Source: City of Hope
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.