Investigators at Memorial Sloan Kettering Cancer Center (MSK) have published results from a clinical trial that found people with recurrent multiple myeloma may benefit from receiving chimeric antigen receptor (CAR) T therapy earlier in the course of their disease.
The study published on February 10, 2023, in The New England Journal of Medicine (NEJM).
The new study was an international phase 3 trial that looked at the effectiveness of the CAR T drug idecabtagene vicleucel (ide-cel, or Abecma) in treating people with multiple myeloma that has come back after other treatments.
The senior author of the NEJM paper is MSK hematologic oncologist Sergio Giralt, MD, Deputy Division Head in the Division of Hematologic Malignancies.
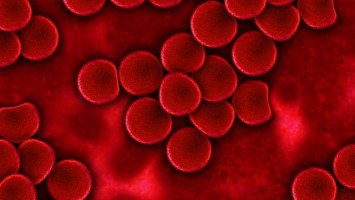
Multiple myeloma is a blood cancer that can be difficult to treat because it develops resistance to drugs.
Recently, CAR T therapy, a type of immunotherapy, has become an important option for people with multiple myeloma.
Here, Dr. Giralt speaks about what the findings mean for people with multiple myeloma.
MSK researchers have played a pivotal role in developing CAR T therapy for this blood cancer.
In addition to leading many clinical trials, Dr. Giralt, who holds the Melvin Berlin Family Chair in Multiple Myeloma, is also Chief Medical Officer of MSK Direct.
What was the goal of this trial studying CAR T therapy to treat people with multiple myeloma?
We wanted to see if patients would benefit from getting this therapy earlier in the course of their treatment.
Ide-cel was previously approved by the U.S. Food and Drug Administration (FDA) to treat people with multiple myeloma whose cancer has come back four or more times after other treatments.
This study, called KarMMa-3, looked at giving the drug sooner, after patients had failed between two and four other treatments.
We know that the more times a patient’s cancer comes back, the harder it is to treat.
KarMMa-3 was a randomised, phase 3 trial that included patients in the United States, Canada, and Europe.
Two-thirds of the patients received ide-cel and one-third received standard care, which consisted of a monoclonal antibody drug, a proteasome inhibitor, or chemotherapy.
What were the findings from this ide-cel clinical trial for recurrent multiple myeloma?
We were very impressed with the results. Compared with standard treatment, there was a nearly sevenfold increase in complete remission rates — meaning that no cancer could be detected in the body after the treatment.
We also looked at how long it took for patients’ cancers to come back after treatment.
One difference in this trial compared with other studies is that patients in the standard treatment group were also able to receive ide-cel — after their other treatment stopped working.
This was great for the trial participants, because they had the opportunity to benefit from this drug no matter to which group they were assigned.
But it also means that it will be hard for us to find out if patients on ide-cel survive longer than with standard treatment alone, because almost everyone eventually got the ide-cel.
What were the side effects from ide-cel?
Severe side effects were experienced in 93% of the people who got ide-cel, compared with 75% of those who got other treatments.
The most common side effect in the ide-cel group was cytokine release syndrome (CRS), which 88% experienced.
This was not surprising to us.
CRS occurs when the T cells release a large amount of proteins called cytokines into the bloodstream.
CRS can be life-threatening, but as one of the first hospitals to regularly offer CAR T therapy, MSK has a great deal of experience helping patients cope with it and with other side effects of this immunotherapy.
How does ide-cel work?
Like other CAR T therapies, ide-cel is a “living drug” that uses a person’s own cells to fight the cancer.
A type of white blood cells called T cells are removed from the patient through a vein.
These T cells are engineered to be able to recognise cancer cells.
The engineered cells are grown in large numbers.
They are then given back to the patient, so they can seek out and destroy the cancer.
In the case of ide-cel, the T cells are engineered to recognise a protein called BCMA.
This protein is found in the cancer cells of people with multiple myeloma.
What does this trial mean for the prognosis (outcome) of people with multiple myeloma?
Right now, ide-cel is FDA-approved only for patients who have had more than four other treatments.
But we hope that it will lead to changes that allow more patients to receive this drug earlier.
Researchers at MSK are continuing to study ide-cel in other settings, including giving it to patients before autologous stem cell or bone marrow transplants (BMTs) to help make these transplants more effective and longer lasting. [“Autologous BMTs” use a patient’s own blood stem cells.]
Can multiple myeloma be cured?
Survival for multiple myeloma has increased tremendously in the past two decades, from an average of 3 or 4 years to more than 10 years.
This is thanks in large part to autologous BMTs, drugs like thalidomide and lenalidomide, and drugs called proteasome inhibitors.
Today, a significant proportion of patients do not have to deal with their disease at all for up to 10 years after their diagnosis and first treatment.
But the disease usually does come back.
I tell my patients that right now our focus is on giving them the longest life possible with the greatest quality of life.
My goal is to get them into a deep remission, so that the cancer doesn’t hurt them and hopefully they never have to deal with it again.
We want to give our patients a long, fruitful, and satisfying life with the minimum burden of treatment.
The entire multiple myeloma team at MSK is focused on these efforts.