In an early-phase trial, nearly three-quarters of patients who received talquetamab, a first-in-class experimental immunotherapy for multiple myeloma, saw a significant reduction in cancer burden within a few months. The study participants had all been previously treated with at least three different therapies without achieving lasting remission, suggesting talquetamab could offer new hope for patients with hard-to-treat multiple myeloma.
“This means that three-quarters of these patients are looking at a new lease on life,” said Ajai Chari, MD, of The Tisch Cancer Institute at Mount Sinai in New York. “We’re hoping that this will soon become available so that patients can benefit.”
Talquetamab binds to both T cells and multiple myeloma cells. This activates an immune response to destroy myeloma cells by bringing T cells to the cancer, a strategy that researchers described as “bringing your army to the enemy.” It also uses a different target than other approved therapies; in this case, the target is a receptor expressed on the surface of cancer cells known as GPRC5D.
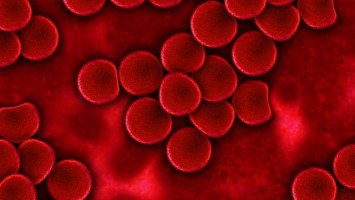
Multiple myeloma is a blood cancer that forms in plasma cells. Several treatments are available, but the prognosis can be very poor and many patients survive less than a year if the disease doesn’t respond to therapy or returns after several different treatments.
The study enrolled a total of 288 patients who were unable to tolerate existing therapies or showed disease progression after at least three multiple myeloma therapies.
After an initial phase generated encouraging results in terms of safety and efficacy, researchers began enrolling additional patients to assess the agent’s efficacy with two different dosing regimens—0.4 mg/kg weekly and 0.8 mg/kg every other week.
Data from patients who had received these same dosing regimens in the first phase were included in the analysis for the second phase.
Seventy-four percent of those receiving 0.4 mg/kg of talquetamab weekly and 73% of those receiving 0.8 mg/kg every other week saw a measurable improvement of their cancer following treatment, the primary endpoint for the trial’s second phase.
More than 30% of patients in both groups had a complete response (no detection of myeloma-specific markers) or better and nearly 60% had a “very good partial response” or better (indicating the cancer was substantially reduced but not necessarily down to zero).
The median time to a measurable response was approximately 1.2 months in both dosing groups and the median duration of response is 9.3 months to date with weekly dosing.
Researchers continue to collect data on the duration of response in the group receiving 0.8 mg/kg every other week and for patients in both dosing groups who had a complete response or better.
Side effects were relatively frequent but typically mild. About three-quarters of patients experienced cytokine release syndrome (a sign of immune activation common with therapies that redirect T cells, typically causing a fever); 60% experienced skin-related side effects such as rash; about half reported taste changes; and about half reported nail disorders. Researchers said 5-6% of patients stopped talquetamab treatment early due to side effects.
The response rate observed in this cohort, which Dr. Chari explained is higher than that of most currently accessible therapies, suggests talquetamab could offer a viable option for patients with hard-to-treat myeloma, offering a chance to extend patient lifespans.
In a separate cohort, 51 patients who had previously received therapies that redirect T cells showed a response to talquetamab. In addition, several other studies are underway to assess the use of talquetamab in combination with other existing and investigational multiple myeloma therapies, which could allow patients to have similar or improved benefits, potentially in earlier stages of treatment.
This study was funded by Janssen Research & Development LLC.
Source: ASH