Treatment with the FLT3-targeted therapeutic gilteritinib (Xospata) improved survival for patients with relapsed or refractory acute myeloid leukaemia (AML) harboring a FLT3 mutation compared with standard chemotherapy regimens, according to results from the ADMIRAL phase III clinical trial presented at the AACR Annual Meeting 2019, March 29-April 3.
Gilteritinib was approved by the U.S. Food and Drug Administration (FDA) for treating adult patients who have relapsed or refractory AML that tests positive for a FLT3 mutation in November 2018.
"The FDA approval of gilteritinib was based on safety data and an interim analysis of the rate of response to gilteritinib in the ADMIRAL trial; it was not based on a comparison of the efficacy of gilteritinib relative to standard chemotherapy," said Alexander E. Perl, MD, associate professor in the Division of Hematology/Oncology at the Perelman School of Medicine at the University of Pennsylvania, and a member of the Abramson Cancer Center.
"We are now presenting the final analysis of the results from the ADMIRAL trial, including data showing that gilteritinib is superior to standard chemotherapy, as measured by improved overall survival."
"These survival data combined with gilteritinib's relatively low toxicity establish gilteritinib monotherapy as the new standard of care for patients with relapsed or refractory FLT3-mutated AML," continued Perl.
"In addition, the relatively low toxicity of gilteritinib and the fact that it is an oral therapy means physicians can manage patients in the outpatient setting, which is a paradigm shift for the treatment of this disease."
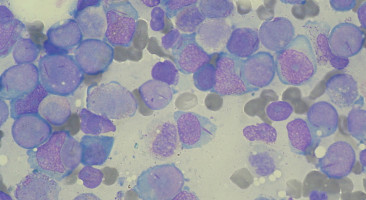
Perl explained that the FLT3 gene is mutated in about one-third of the AML cases diagnosed in the United States. Patients with relapsed or refractory FLT3-mutated AML have a particularly poor prognosis, with standard chemotherapy regimens yielding low remission rates and any remissions achieved lasting a short duration, he said.
ADMIRAL was a randomized, phase III clinical trial designed to determine whether gilteritinib improved survival for patients with relapsed or refractory FLT3-mutated AML compared with standard chemotherapy regimens, which included investigator's choice of low-dose cytarabine; azacitidine; mitoxantrone, etoposide, and cytarabine; and fludarabine, cytarabine, granulocyte colony-stimulating factor, and idarubicin.
Of the 371 patients enrolled in the clinical trial, 247 were randomly assigned to gilteritinib and 124 to standard chemotherapy.
At the final analysis, patients assigned gilteritinib were found to have a 36 percent reduction in risk of death compared with those assigned standard chemotherapy.
Median overall survival was 9.3 months for those assigned gilteritinib versus 5.6 months for those assigned standard chemotherapy.
At 12 months, 37.1 percent of the patients treated with gilteritinib were alive compared with 16.7 percent of those assigned standard chemotherapy.
The combined rate of complete remission (which means a patient has no evidence of disease with full recovery of blood counts) and complete remission with partial hematologic recovery (which means a patient has no evidence of disease with partial recovery of blood counts) was 34.0 percent for those assigned gilteritinib and 15.3 percent for those assigned standard chemotherapy.
"The longest survival in the gilteritinib arm was seen among patients who proceeded to transplant and then resumed gilteritinib thereafter to prevent relapse, but unfortunately long-term survival was very uncommon on either treatment arm," said Perl.
"In an effort to further improve long-term outcomes, clinical trials testing gilteritinib in combination with other therapies for relapsed or refractory FLT3-mutated AML and testing gilteritinib as frontline therapy for newly diagnosed patients have already been launched."
According to Perl, the main limitation of the study is that the standard frontline treatment for FLT3-mutated AML changed during enrollment to the ADMIRAL trial because the FDA approved the FLT3-targeted therapeutic midostaurin for this indication in April 2017; thus, a small minority of patients in both arms received prior FLT3-targeted therapy. It is possible that leukaemias that relapsed after or were refractory to frontline treatment that included midostaurin were less dependent on FLT3 for their growth and therefore had less likelihood of responding to gilteritinib, he explained.
Watch Prof Perl's interview with ecancer at AACR 2019 here.
Source: AACR
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.