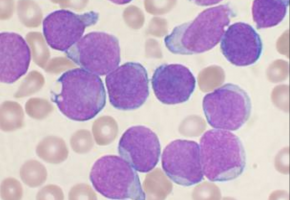
The human gene MLL is named for the mixed lineage leukaemia it creates.
Specifically, the gene may break apart and fuse with parts from one of a number of other genes on other chromosomes to create cancer-causing translocations.
These translocations make new proteins that have never been seen by the cell and can cause cancerous growth.
In addition to mixed lineage leukaemia which occurs in children, MLL translocations cause about 15 percent of adult acute myeloid leukaemia (AML).
Thus MLL has been a major focus of drug development aimed at stopping the cancers caused by these translocations.
However, despite their promise, these drugs have struggled to show clinical benefit.
A University of Colorado Cancer Center paper published in the journal Cancer Cell challenges existing understanding of potential therapeutic targets in MLL-translocation leukemia.
Specifically, the study shows that within the family of MLL-related proteins, MLL2 and not MLL is the most appropriate target for drugs challenging the disease.
In other words, drug developers aiming at MLL may have been missing slightly to one side of the real target.
The finding stems from the fact that in these cases of leukemia associated with MLL, only one of the two copies of the gene is altered, meaning that MLL translocations exist alongside the unaffected copy.
Previous work had shown that these unaffected copies of MLL - what researchers call the wildtype form of the gene - were working with MLL translocations to cause cancer.
This finding formed the basis for drug development directed at wildtype MLL.
First author of the current paper, Yufei Chen, PhD, describes her early work in this landscape: "When I started my work, there were already a number of studies showing that MLL is very important to maintain this type of leukaemia. I wanted to see if I could repeat these findings in a knockout mouse by deleting MLL. But I couldn't see any difference between the control and the knockout."
Basically, the existence of wildtype MLL seemed to make no difference to the development of leukaemia in these mice.
Medicinal chemists had been trying to silence this remaining unaltered and supposedly dangerous MLL, but why would it be worth developing a drug against a target whose removal has no effect on the disease?
Of course, Chen was initially skeptical of her results.
Surely artifacts of her execution (aka "mistakes") explained her inability to replicate the results of these widely-respected previous studies.
Working in the lab of Patricia Ernst, PhD, CU Cancer Center investigator and Professor of Pediatrics and Pharmacology at the CU School of Medicine, Chen, "repeated the experiment, like, a million times," she says.
Every time, she got negative results: The silencing of wildtype MLL had no effect on the development of leukemia.
Also collaborating on the project was lab assistant Jasmine Lee, undergraduate at UC Denver.
If it wasn't experimental procedure, perhaps it was the specific mouse model?
To rule out this possibility, Chen got another MLL knockout model from German collaborator A. Francis Stewart, PhD, professor of Genomics and director of the Biotechnology Center (BIOTEC) at Technische Universitat Dresden.
"International collaboration made this work possible," Ernst says. "Nobody really goes through the trouble of confirming their results in a second mouse model, but Yufei did it just to be 110 percent sure."
Gene knockout in this German model meant the total loss of MLL protein.
And yet Chen got the same result: There was no difference in the development of leukaemia between mice retaining MLL and the new model that lacked it.
"We started with something that was considered established fact, namely that wildtype MLL contributed to MLL translocation leukaemia. Then we overturned it," Ernst says. "Still, all this negative data was difficult to explain and we wondered if there was more to the story."
To Chen and Ernst, there was something going on in this mix of MLL translocations with MLL wildtype genes.
Maybe there was another partner involved?
"MLL2 is the most closely related protein to MLL. Some studies suggest that most of the time, MLL and MLL2 have distinct functions. But we wondered if these related genes might be somehow covering for each other," Ernst says.
The group was going to need more mouse models.
In addition to their MLL knockout, "We got MLL2 knockout and double knockouts," Chen says. At the Functional Genomics Shared Resource at the CU Cancer Center, Chen worked with manager Molisheree Joshi, PhD to recreate these knockouts in human cells as well.
Again, when they knocked out MLL, there was no change in the course of leukaemia.
But when they knocked out MLL2, it resulted in about 40 percent less leukaemia.
And when they knocked out both MLL and MLL2, they saw about 90 percent reduction in leukaemia.
Finding that MLL2 may be a target in MLL-translocation leukaemia was an important result.
But the question of MLL involvement that the group thought it had put to rest (namely the finding that there was no involvement) had now acquired an important nuance: "How can a thing that does nothing on its own - namely MLL knockout - have such a dramatic effect when combined with this other thing, namely MLL2 knockout?" Chen asks.
"It's a classic synergism," Ernst says. "Like in a car: if you mess with the brakes a little, maybe nothing happens. But if you mess with the brakes a little and also mess with the accelerator so that it sticks, now you've got a problem."
Chen took MLL2 knockout leukaemia cells to the CU Cancer Center Genomics and Microarray Core Facility to see if she could figure out why the gene collaborated with MLL translocations (and with wildtype MLL) to cause leukaemia.
Basically, RNA sequencing could tell her how MLL2 was connected to other genes - what did it turn up or down, and what general pathways did MLL2 influence?
It turned out that 177 genes were deregulated by MLL2 alone and that 444 genes were deregulated when both MLL and MLL2 were removed.
When viewed together, it turned out that groups of these genes had very significant meaning in the context of leukaemia, including members of three leukaemia pathways that are already considered significant drug targets in AML.
"These are all very important leukaemia pathways," Ernst says. "If you had a drug for MLL2, you could hit these really big targets."
Additionally, while MLL is essential to the function of healthy bone marrow stem cells, MLL2 seems to have little function in the adult body.
This means that targeting MLL2 may come with fewer side effects.
Of course, the group's continuing work is making the case for the development of exactly this kind of drug.
Chen is working with cells from human cancer patient samples provided by CU Cancer Center investigator Daniel Pollyea, MD and Children's Colorado investigator Kelly Maloney, MD, to show that the effect of MLL2 inhibition is not specific to mouse biology.
And Ernst is working to show how broadly relevant MLL2 as a drug target may be in other blood cancers.
According to Ernst, this study exemplifies the results that can come from utilizing the full technological resources of a major academic and medical campus, paired with collaboration between investigators across the spectrum of basic to clinical research.
"This is a great example of researchers working together," Ernst says. "This basic science has the real potential to affect the development of future drugs that could improve the lives of patients with these conditions."