Some patients with relapsed or treatment-resistant acute myeloid leukaemia, a form of blood cancer for which there are few treatments, may achieve remission with an experimental targeted therapy, according to early trial data published online in Blood, a Journal of the American Society of Hematology (ASH).
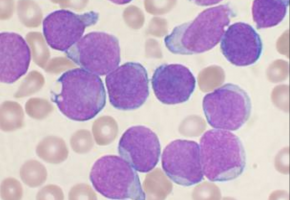
Up to 15 percent of people with AML have a mutation in the IDH2 gene, which prevents their white blood cells from maturing into neutrophils, an integral part of the body’s immune system.
Instead, these white blood cells become leukaemia cells.
Unlike standard AML therapies, which aggressively target all white blood cells, the experimental therapy enasidenib inhibits the mutated IDH2 gene, allowing immature white blood cells to naturally mature into neutrophils.
“Instead of killing the rampant white blood cells, this therapy is designed to turn them into normal, healthy cells,” said study author Eytan Stein, MD, of Memorial Sloan Kettering Cancer Center in New York.
Of the 239 IDH2 mutation positive AML patients included in this trial, 74 percent had treatment-resistant disease with few or no remaining therapy options available.
Of those 176 patients, 71 (40.3%) responded, with 34 (19.3%) achieving complete remission.
At data cut-off, patients who achieved a partial response survived a median of 14.4 months, while those who achieved complete response attained 19.7 months.
Further data collection on these patients will be included in future studies.
Overall survival for this group nearly tripled compared to previous studies evaluating other treatments in this patient population, up from 3.3 months to 9.3 months.
“In this early study, the survival benefit of nine months in patients with advanced relapsed or treatment-resistant disease is very significant,” noted Dr. Stein. “We are further encouraged to see that there we so few serious adverse events for these patients.”
Adverse events included increased bilirubin, nausea, IDH-DS (a buildup of fluid in the body and/or lungs), and a proliferation of white blood cells known as leukocytosis.
Two participants who experienced IDH-DS died in the course of treatment.
Further trials to assess enasidenib as a frontline therapy, in combination with standard AML treatments, and in treating other mutant IDH2 disorders like myelodysplastic syndrome (MDS) are planned or are ongoing.
Source: Blood