It's not often that a fall saves someone's life.
Helen Powell, 74, says that was the case for her.
A computerised tomography scan that followed her fall revealed a cancerous brain tumour that led her to Mayo Clinic and surgery using first-in-the-world technology.
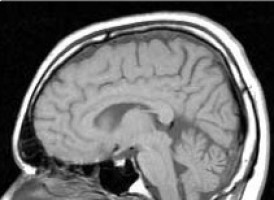
Brain magnetic resonance elastography (MRE) imaging, showed the precise firmness of her tumour.
New slip interface imaging further revealed how attached the tumour was to normal brain tissue -- even before starting surgery.
The imaging techniques, invented and available only at Mayo Clinic, show whether the tumour is soft and can be removed easily, or if it is firm, making surgery more challenging and time consuming.
"Brain magnetic resonance elastography and slip interface imaging help avoid surprises in surgery that could lead to complications for the patient," says Jamie Van Gompel, M.D., a neurosurgeon at Mayo Clinic. "Once in surgery, we may find a tumour is stiffer than expected and will take more time to remove than we had planned, or alternatively, we may find the tumour to be more adherent to brain than anticipated, raising the risk of a complication from that surgery.
"Slip interface imaging provides information on the interface between the tumour boundary and surrounding tissue. This interface can be capsule-like in which the tumour slides or slips within the surrounding normal tissue, or it can form a rigid connection in which the tumour is fixed to the surrounding tissue. Surgeons use the images to plan the proper time and the safest method for extraction. This technology allows us to get a feel for the tumour without opening someone's head and this will really impact patient safety," says Dr. Van Gompel.
New Mayo Clinic research, published in the Journal of Magnetic Resonance Imaging, confirms the effectiveness of slip interface imaging.
The study looked at the level of tumour adhesion in 25 patients.
The brain magnetic resonance elastography and slip interface imaging showed 16 patients had tumours that could be easily removed; nine patients had tumours with adhesion to the brain; and six were mixed.
Physicians found all the pre-surgical images to be an accurate assessment of the tumours and therefore an invaluable surgical planning tool.
"Slip interface imaging gives Mayo Clinic physicians new information that allows an individualised approach to tumour surgery for both cancerous and noncancerous lesions. If a tumour is soft, it can sometimes be sucked out. If it is firm, it may need ultrasonic extraction. Before we had this imaging capability, it was not uncommon to find unexpected risks that required follow up surgery," says John Huston III, M.D., a radiologist who helped develop the imaging technology.
In Helen Powell's case, slip interface imaging helped her surgeon determine that despite having a challenging, firm tumour, he could remove most of it in one surgery and attack the rest with radiation. And, he could extract it through her nose rather than performing a craniotomy.
That cut risk of rare but also significant potential complications like stroke or blindness.
For Powell, it was an answer to her prayers.
For 3½ years before her diagnosis at Mayo Clinic, no doctor or medical center could figure out what was wrong.
She suffered constant shoulder and joint pain, was nauseated most of the time and was slowly losing her eyesight.
After surgery, she noticed a dramatic change.
"When I woke up, I could see again. My shoulders didn't hurt anymore and I didn't have any more joint pain. I could walk and think again. It was a miracle," she says.
Source: Mayo Clinic
The World Cancer Declaration recognises that to make major reductions in premature deaths, innovative education and training opportunities for healthcare workers in all disciplines of cancer control need to improve significantly.
ecancer plays a critical part in improving access to education for medical professionals.
Every day we help doctors, nurses, patients and their advocates to further their knowledge and improve the quality of care. Please make a donation to support our ongoing work.
Thank you for your support.