by ecancer reporter Janet Fricker
A rapid, cheap and ultrasensitive blood test distinguishing pancreatic cancer from pancreatitis is reported in Nature Biomedical Engineering.
Despite the dire prognosis of pancreatic cancer, characterised by aggressive local invasion, early metastasis, and high rates of therapy resistance, there are currently no FDA-approved non-invasive diagnostic assays.
To reduce cancer morbidity and mortality noninvasive biomarkers discriminating between pancreatic cancer and chronic pancreatitis are desperately needed.
In the current article, Ye Hu and colleagues, from Houston Methodist Research Institute, Texas, describe their new assay that is capable of quantifying tumour-derived extracellular vesicles (EVs) from as little as 1 µl of plasma.
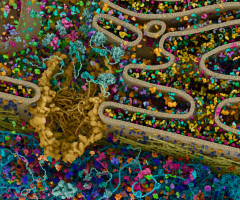
EVs, including exosomes and other membraneous vesicles, are excreted into the extracellular space by most cells, from where they then accumulate in the circulation.
While EVs are known to actively participate in tumour initiation, progression and metastasis, translating tumour EVs into cancer biomarkers has proved challenging due to difficulties distinguishing tumour-derived EVs from normal EVs.
For the current study, the team adopted a different approach of quantifying EVs associated with specific disease states.
Investigating 128 different membrane proteins, they found that only the EV biomarker ephrin type-A receptor2 (EphA2) exhibited significantly higher expression in human pancreatic cancer tissue samples than chronic pancreatitis or normal pancreatic tissue samples.
In a pilot study, the team analysed EphA2 signals in 48 healthy controls, 48 patients with pancreatitis and 49 patients with pancreatic cancer (stage I-III).
The assay used the binding of antibody-conjugated gold nanospheres and nanorods to EVs captured by EV-specific antibodies on a sensor chip to produce a local Plasmon effect that enhances tumour derives EV detection sensitivity and specificity.
Results showed that EphA2-EV for pancreatic cancer versus normal controls had a sensitivity of 94% and a specificity of 85%; and that EphA2-EV for pancreatic cancer versus pancreatitis had a sensitivity of 89% and a specificity of 85%.
“These results indicate a strong association between circulating EphA2-EV and pancreatic cancer, including early-stage pancreatic cancer, suggesting the potential utility of EphA2-EV as an early detection marker,” write the authors.
While pancreatic cancer was selected as a proof-of-principal model the approach, suggest the authors, could be readily customized to diagnose and monitor other cancers and infections.
The potential for EphA2-EV to detect other forms of cancer, they add, should be addressed in future studies.
We are an independent charity and are not backed by a large company or society. We raise every penny ourselves to improve the standards of cancer care through education. You can help us continue our work to address inequalities in cancer care by making a donation.
Any donation, however small, contributes directly towards the costs of creating and sharing free oncology education.
Together we can get better outcomes for patients by tackling global inequalities in access to the results of cancer research.
Thank you for your support.